Migraine epidemiology: In pregnancy and postpartum
Migraine is generally known to affect mostly women with the peak incidence occurring in the reproductive years.1 As part of the “Headache and Pain 1 session” at the 7th Congress of the European Academy of Neurology (EAN), Dr. Nirit Lev (Meir Medical Center, Kfar Saba, Tel Aviv, Israel) provided clinical evidence of migraine epidemiology in women during and after pregnancy while considering their characteristics and medical needs.
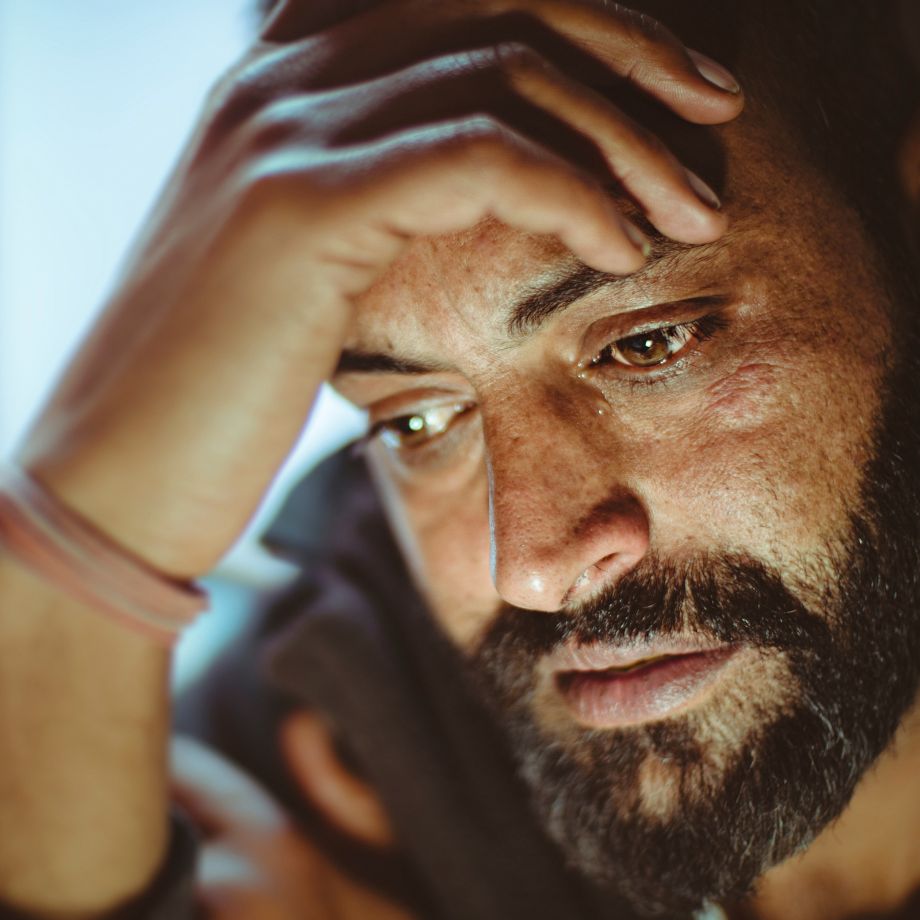
When we are following a pregnant woman with migraine, we need to look at the whole picture; not only at her migraine, not only [at] her pregnancy.
The prevalence of migraine in pregnancy
Dr. Nirit Lev started her presentation by mentioning that with the onset of puberty, the prevalence of migraine becomes three times more common in women than in men.1 In contrast, men have a relatively stable course of migraine throughout their lifespan.1 She reported that females with migraine experience an overall improvement in migraine symptoms during pregnancy, especially in the second and third trimester.1 She further explained that the remission of migraine symptoms in women during pregnancy parallels the increased estrogen and progesterone levels during pregnancy.2 Nevertheless, Dr. Lev indicated that there were a minority of women that reported worsening of migraine during their pregnancy; some even experienced de novo migraine symptoms during the first trimester of their pregnancy.
Women with migraine during pregnancy
In the next segment of her talk, Dr. Lev presented results based on a study that was conducted using an electronic health record database. She stated that 145,102 women who gave birth during a period of six years (2014–2020) were included in the study. According to Dr. Lev, over 10,000 pregnant women had a diagnosis of migraine without aura, while 1,576 pregnant women experienced migraine with aura. She indicated that pregnant women with migraine had an overall higher risk of obstetric complications such as gestational diabetes, hyperlipidemia, preeclampsia, and blood clots, along with psychiatric concomitant diseases like depression compared to pregnant women without migraine. Furthermore, Dr. Lev reported that pregnant women with migraine seek more medical consultations, had more visits to the emergency department and consumed more medications in comparison to women without migraine. Lastly, Dr. Lev indicated that there was a higher incidence of preterm deliveries and a lower number of live born infants in women with migraine as compared to women without migraine.
Women with migraine in the postpartum period
Dr. Lev then discussed the clinical evidence of women with migraine during the postpartum period, reporting that women with migraine seek more medical consultations, had more laboratory examinations and more brain imaging studies than women without migraine. In Dr. Lev’s opinion, pregnant women with migraine should be included in a high-risk pregnancy protocol of care throughout their pregnancy as they were shown to be at a higher risk of having obstetric and medical complications compared with women without migraine. She also emphasized that a specialized neurological follow-up visit, in addition to obstetrics and gynecology, should be provided to women with migraine during the pregnancy and postpartum period. Dr. Lev concluded by stressing that “managing migraine in pregnancy is more complicated and needs special attention and expertise.”
Todd C, Lagman-Bartolome AM, Lay C. Women and Migraine: the Role of Hormones. Current Neurology and Neuroscience Reports 2018;18:42.
Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis--part I. Headache 2006;46:3-23.