Vascular changes in migraine
Migraine has a significant impact on patients’ lives but we are still unravelling the mechanisms behind this disabling condition. Watch the short clip below to find out more about the latest research into the events leading up to and during a migraine attack, and especially the role of vasodilation, as demonstrated using sildenafil and CGRP (calcitonin gene-related peptide).
Still want to find out more? Further information on the pathophysiology of migraine is available in the migraine knowledge hub.
Transcript
Affecting around 10% of the adult population worldwide, migraine is the second most prevalent neurological disorder and the leading cause of disability in under 50s but what causes this complex, multifactorial neurological disorder?1
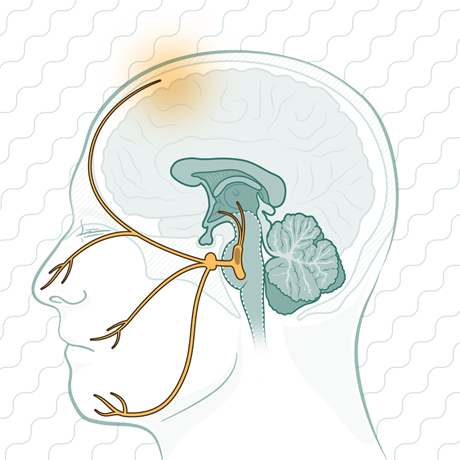
The exact mechanisms underlying the onset of a migraine attack remain unclear, but research continues to unravel the structures and pathways involved, including complex bidirectional cross-talk between cranial blood vessels and their trigeminal nerve endings.1
Development of the excruciating throbbing headache of migraine requires the initial activation and increased sensitization of trigeminal nociceptive afferents that innervate the cranial meninges and their related large blood vessels.1
The cranial meninges are comprised of two layers: the dura mater, which is highly vascularized, and the leptomeninges.1 Accumulating evidence implicates vasodilation of meningeal blood vessels in the development of migraine1-6:
- Researchers in Denmark have shown that sildenafil can provoke migraine symptoms, as can CGRP2
- In healthy volunteers, sildenafil administration was associated with a significant increase in diameter of extracranial and intradural middle meningeal arteries vs saline administration2
- Sildenafil, a phosphodiesterase type 5 (PDE5) inhibitor, protects cyclic guanosine monophosphate (cGMP) from degradation by PDE5, indirectly allowing smooth-muscle relaxation and vasodilation due to increasing cGMP levels in response to nitric oxide (NO) binding to guanylate cyclase receptors2
- In healthy volunteers, sildenafil administration was associated with a significant increase in diameter of extracranial and intradural middle meningeal arteries vs saline administration2
- Similar results were seen following administration of CGRP, a neuropeptide with roles in vasodilation, neurogenic inflammation, and peripheral sensitization2
- Consistent with these findings, earlier studies found that exogenous CGRP infusions triggered delayed migraine-like headaches accompanied by a unilateral dilation of the middle meningeal artery, but no dilation of the middle cerebral artery, suggesting a peripheral role for CGRP1,3,4
- The role of other potential vasodilators, including vasoactive intestinal peptide (VIP),1 endothelin,5 and serotonin (5-hydroxytryptamine)6 in migraine pathophysiology has also been investigated, with mixed results, which is also congruent with the notion that intracranial vasodilation alone is not sufficient to activate meningeal afferents and trigger migraine1
Clearly, there is much still to be learned about migraine pathophysiology, especially the initiating processes, but the knowledge that we have gained to date is already resulting in clinically relevant improvements in the management of this disabling condition. 1–6
Levy D, Labastida-Ramirez A, MaassenVanDenBrink A. Cephalalgia 2018;epub ahead of print.
Christensen CE, Amin FM, Younis S, Lindberg U, de Koning P, Petersen ET, Paulson OB, Larsson HBW, Ashina M. Cephalalgia 2018;epub ahead of print.
Hansen JM, Hauge AW, Olesen J, Ashina M. Cephalalgia 2010;30:1179–1186.
Asghar MS, Hansen AE, Amin FM, van der Geest RJ, Koning Pv, Larsson HB, Olesen J, Ashina M. Ann Neurol 2011;69:635–645.
Iljazi A, Ayata C, Ashina M, Hougaard A. Curr Pain Headache Rep 2018;22:27.
Deen M, Hougaard A, Hansen HD, Svarer C, Eiberg H, Lehel S, Knudsen GM, Ashina M. Cephalalgia 2018;epub ahead of print.