Types of headache and migraine
There are many different types of migraine and headache – the International Classification of Headache Disorders (ICHD) lists more than 200 varieties of these disorders.1
The classification and diagnosis of headache disorders
Given the wide range of different headache and migraine types, systematically classifying and diagnosing them have been deemed essential to aid proper clinical management.2 The third edition of the ICHD is the current standard for headache classification and diagnosis.1 The classification of headache types is hierarchical, and a detailed diagnosis requires navigating the diagnostic criteria of the subtypes and subforms.1 Additionally, a detailed history of the patient’s headache is crucial for forming a correct diagnosis.3 This should include details such as headache frequency, duration, character, severity, location, quality, triggering and aggravating factors, alleviating features and age of onset. Additional details such as lifestyle habits and comorbid conditions, or underlying medical disorders, are also useful for aiding a diagnosis.3
While the symptoms and features of different headache types vary, there is also significant overlap among them, making an exact diagnosis a challenge. Moreover, patients can experience different headache types, which necessitates multiple diagnoses.1 To make matters even more difficult, a headache’s symptoms, pain intensity and duration can vary greatly, even within the same patient.
Headache types
There are two main categories of headache disorders: primary headaches and secondary headaches.1 While a primary headache is a disorder of its own, a secondary headache is only a symptom of an underlying condition. Primary headaches can be further categorised into 4 main types: 1) migraine, 2) tension-type headache (TTH), 3) trigeminal autonomic cephalalgias (TACs) such as cluster headache, and 4) other primary headache disorders.1
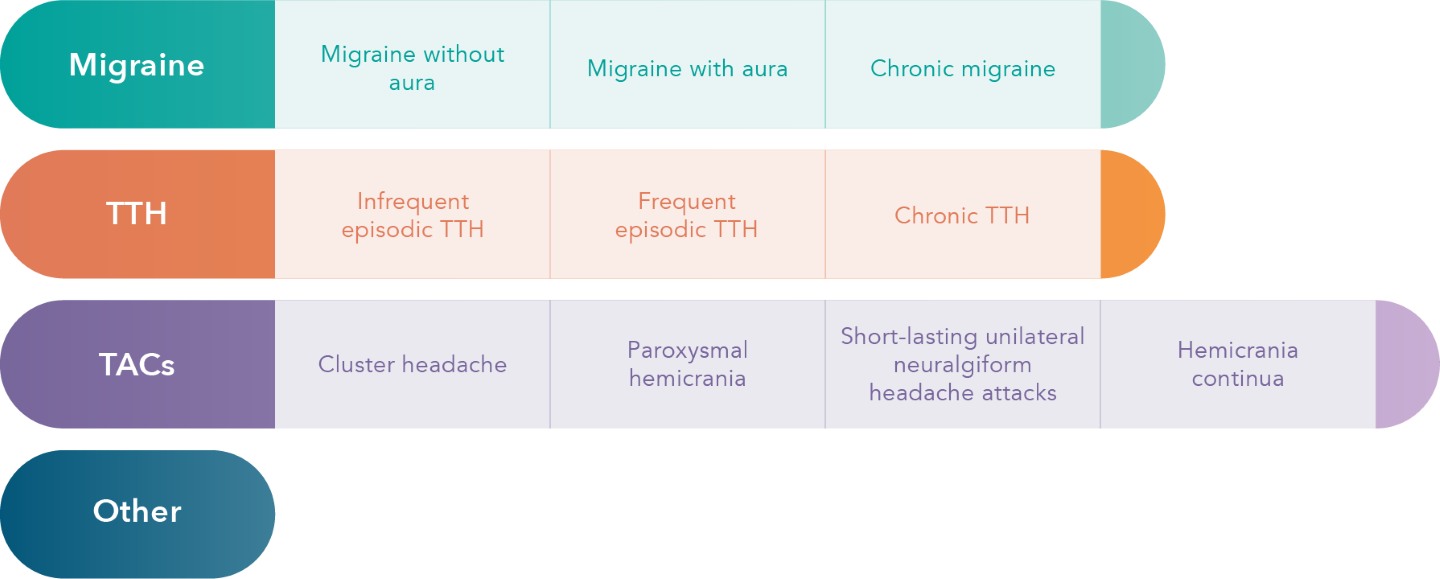
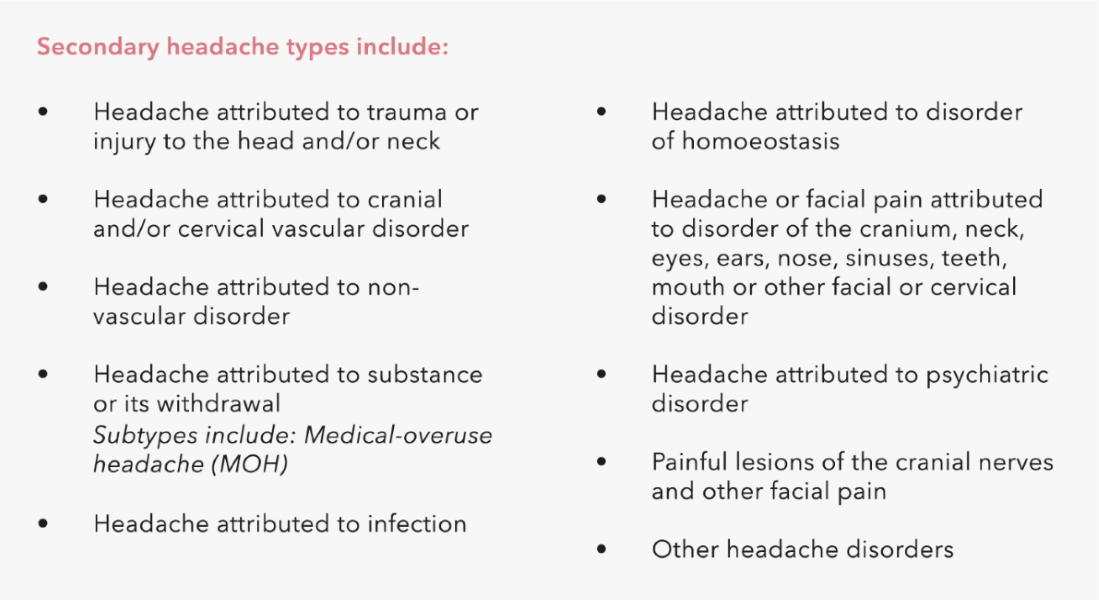
Meanwhile, secondary headaches can be attributed to events like trauma or injury, cranial or vascular disorders, infection or substance use such as medication-overuse headache (MOH).1
Primary headaches constitute the large majority of all headache disorders (more than 95%), of which tension-type headache is the most common.4 (Figure 1). According to the World Health Organization (WHO), the most common secondary headache is MOH.5
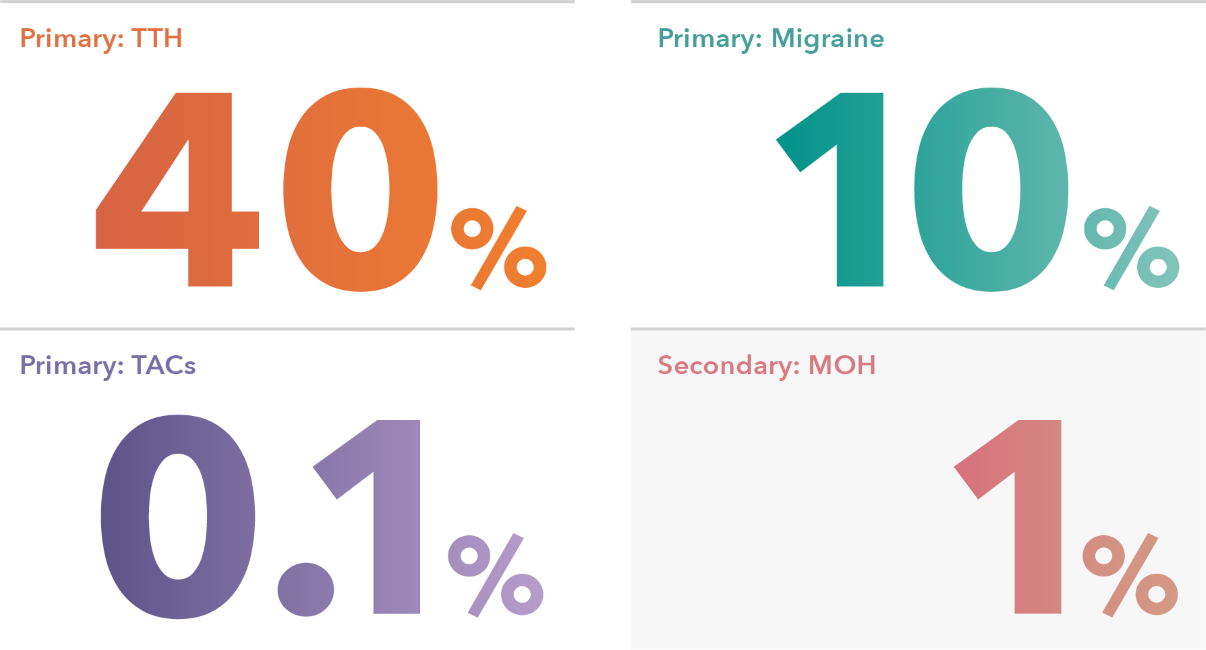
Figure 1. Global prevalence of headache disorders3,6
Primary headaches
Primary headaches, TTH and migraine in particular, are extremely prevalent and a huge burden to the society.7,8 Although TTH is more common than migraine, the greater disability weight of migraine gives it a higher years lived with disability (YLD) score compared to TTH.7,8 In fact, migraine has been ranked as the leading cause of disability (measured in YLD) among individuals aged 15–49 years.7
Migraine
The two major types of migraine are migraine without aura (formerly called common migraine) and migraine with aura (also called classic migraine).1 Attacks of migraine without aura usually last 4–72 hours. Typical features include unilateral, pulsating headache of moderate to severe intensity associated with nausea, vomiting and sensitivity to light, sound or smell.1 Migraine with aura starts with aura symptoms preceding the actual headache, lasting up to one hour.1 Both of these migraine types are characterised as episodic migraine, based on the number of headache days per month. If a migraine occurs on 15 or more days per month for more than three months, it is instead classified as a chronic migraine.1 Although chronic migraine is less common than episodic migraine – affecting approximately one tenth of all migraineurs – it is extremely disabling and severely impacts the patient’s quality of life.9
Tension-type headache (TTH)
TTH is typically not as severe as migraine.3 It is often a dull, bilateral, mild-to-moderate headache pain without other striking features.3 The infrequent episodic form of TTH is thought to be experienced by almost everyone at one point or other, and generally does not require any medical attention.1 Frequent episodic TTH, on the other hand, is more disabling and may warrant medication, whereas the rarer chronic TTH is severely disabling, usually leading to a greatly decreased quality of life.1

Trigeminal autonomic cephalalgias (TACs)
TACs are a group of primary headaches that share the clinical features of a unilateral headache and are often associated with ipsilateral cranial autonomic features.3 The most common TAC is cluster headache, characterised by clusters of severe attacks that last between 15 min and 3 hours, occurring daily for a few weeks up to a few months.3 The remission period between these clusters can last several months to years.1 Cluster headache, for unknown reasons, affects three times more men than women.1 Other TACs include paroxysmal hemicrania, short-lasting unilateral neuralgiform headache attacks and hemicrania continua.1
Secondary headaches
Unlike primary headaches, secondary headaches are symptoms of underlying conditions or attributed to external factors such as injury, cranial or vascular disorders, infection or substance use.1 Although secondary headaches are uncommon, diagnosing them is important, as timely intervention can be crucial for treating a potentially fatal underlying condition.4 Usually, patients with secondary headaches will have ‘red flag’ symptoms in their patient history that should aid in forming the diagnosis.4
Medication-overuse headache (MOH)
MOH, also known as drug-induced headache or rebound headache, is a type of secondary headache associated with regular overuse of headache medication, and usually develops secondary to a pre-existing headache syndrome that is being treated with medication.1 Virtually all types of headache medication can lead to MOH.6 It has been suggested that MOH has a genetic component.6 Due to a lack of large-scale studies, more research is needed to draw conclusive results.6 Managing MOH is not completely straightforward, as medication withdrawal may not always improve outcomes, instead sometimes even leading to unanticipated negative outcomes.3 However, research suggests that complete withdrawal of the medication that causes MOH is generally more effective than just simply restricting its intake.10
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.
Lipton RB, Bigal ME, Steiner TJ, Silberstein SD, Olesen J. Classification of primary headaches. Neurology 2004;63:427-35.
Rizzoli P, Mullally WJ. Headache. Am J Med 2018;131:17-24.
Ahmed F. Headache disorders: differentiating and managing the common subtypes. Br J Pain 2012;6:124-32.
World Health Organization (WHO). Headache disorders. 2016. (Accessed January 2020, at https://www.who.int/news-room/fact-sheets/detail/headache-disorders.)
Kristoffersen ES, Lundqvist C. Medication-overuse headache: epidemiology, diagnosis and treatment. Ther Adv Drug Saf 2014;5:87-99.
GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2018;17:954-76.
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211-59.
Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia 2015;35:563-78.
Nielsen M, Carlsen LN, Munksgaard SB, Engelstoft IMS, Jensen RH, Bendtsen L. Complete withdrawal is the most effective approach to reduce disability in patients with medication-overuse headache: A randomized controlled open-label trial. Cephalalgia 2019;39:863-72.