
Empowering patients for shared decision-making in managing their migraine
In chronic illness, patient self-management is inevitable as patients make decisions about their condition every day.1 This introduces a new chronic disease paradigm which concerns the patient and healthcare professional relationship and involves collaborative care and self‑management education.1 Clinician-patient communication is important for the effective management of migraine since the self-assessment of headache frequency, severity, and associated impairment can greatly impact treatment selection.2 Currently, most clinician‑patient communications occur through dialogue without the support of relevant migraine self-assessment data.2
Gaps in patient-clinician communication for migraine management
Communication between patients and clinicians often takes place in a time‑constrained environment.2 The strategy and consistency with which the most significant information is elicited during a clinical encounter may not be optimal for guiding effective clinical decision‑making.2 A study of migraine-related communications illustrated how these factors can impact migraine management, finding that clinicians most commonly based their approach to migraine management on attack frequency alone.2 In this study, post-visit interviews with clinicians and patients revealed that 55% of the clinician-patient pairs disagreed on the frequency of headache established during the visit.2 Furthermore, migraine-associated impairment was acknowledged in only 10% of the visits and perceived as being misjudged in 51% of cases.2 Unlike many chronic diseases that have clear and specific diagnostic criteria and measurements, migraine has a less established physiological basis and lacks an exact medical diagnostic measurement. This challenge indicates that the diagnosis and treatment processes for migraine are largely guided by patients’ own description of their symptoms.3 To aid clinician-patient relationships, current health policies emphasize the need for an equitable patient and clinician rapport, which requires a certain level of patient empowerment.4
Empowering migraine patients
By facilitating patient engagement and communication, clinicians can foster patient empowerment and better patient outcomes.4 Empowering patients indicates that the patient accepts responsibility to manage their own condition and are encouraged to solve their problems aided by information from a healthcare professional.1 Empowerment is seen as both a process and an outcome.5 The empowerment process can be divided into two parts: an intra-personal dimension where the patient transforms due to interactive learning, and an interpersonal dimension arising from the relationship between the patient and the healthcare provider.5 Patient empowerment is crucial to shared decision-making, where patients can learn to solve their own problems with information and support from healthcare professionals (Figure 1).6
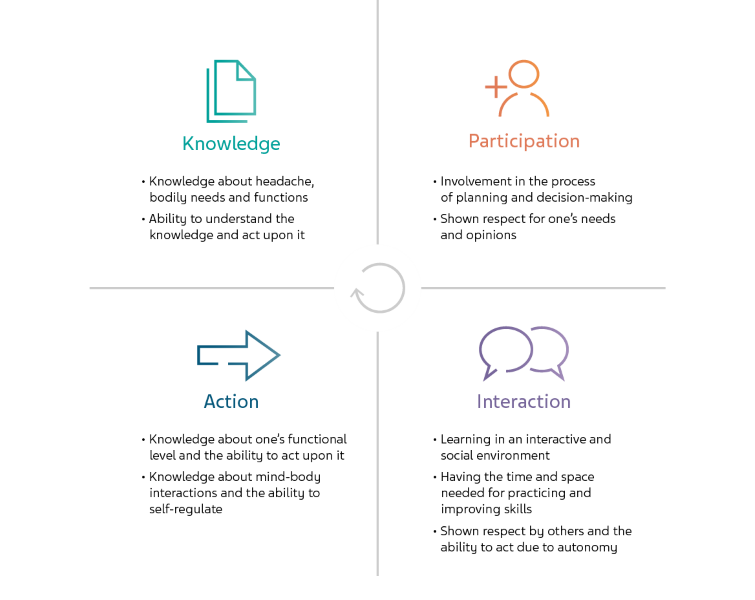
Figure 1. Empowering patient education through knowledge, participation, action and interaction.5
Shared decision-making
An educational partnership is required to support and empower the patient to collaborate, engage, and manage decision-making.5 The patient is empowered to gain knowledge and skills to cope with psychosocial and functional issues, to have the right to self-determination, to mobilize resources to become responsible and efficient in self-management, and to adhere to mutual plans.5 For clinicians, investigating the patients’ perspective of migraine and headache management is the first step to understanding the patients’ current involvement in their own care, to identify areas for patient education and to involve the patients as a resource in managing their headache.1 A qualitative study found that patients’ assigned themselves a central role in their involvement in their headache care, including their role during healthcare consultations and decisions about medication use, eliciting that patients take responsibility for managing their headache.1 The study data also indicated that patients with a shorter headache history, more severe headaches, and greater disability were more self-directed.1 Therefore, patients adapt their headache management to suit their needs and preferences, which makes migraine and headache management highly individualized (see Figure 2).1

Figure 2. Areas of migraine and headache management1
Identifying triggers
Migraine involves an abnormal sensitivity in the brain to various triggers.3 One unique challenge of migraine management lies in the difficulties of diagnosing and treating it, while patients endure extremely painful migraines caused by a wide variety of unknown triggers.3 Thus, there is a critical need for both self-recognition and social recognition in migraine management.3 Migraine sufferers should perform a series of individual tasks to discover and identify their own triggers and find effective coping mechanisms.3 Simultaneously, migraine patients also need to obtain social recognition and help during migraine attacks.3 To effectively manage migraine, most clinicians recommend avoiding triggers. This relies primarily on the patients themselves, in identifying and evading their triggers, rather than seeking action from healthcare providers.3 One study found that the individualized and subjective nature of migraine triggers and symptoms not only made it difficult for participants to recognize their own triggers and symptoms, but also caused significant barriers in seeking professional help.3 Approaches for managing triggers differ widely, but maintaining a healthy lifestyle and learning to cope with triggers remains fundamental in the management of migraine.
Lifestyle management in migraine patients
Empowering patients to modify their lifestyle can reduce both their headache and related comorbidities.7 One study found that empowering patients with chronic daily headache (CDH) to modify their lifestyles resulted in a better Health Promoting Lifestyle Profile (HPLP) score, lower headache intensity, and a significantly lower Depression Anxiety Stress Scales (DASS) score.7 Physicians can help their patients with migraine modify their triggers and mitigate the severity and frequency of their symptoms by offering lifestyle modifications based on SEEDS: sleep, exercise, eat, diary, and stress.8

Sleep
Poor sleep is described as a migraine trigger and those with poor sleep report have lower quality of life.8 Behavioral modification of sleep hygiene can convert chronic migraine to episodic migraine.8 Patients are encouraged to keep the bedroom quiet, dark, and cool, and to go to sleep at the same time every night.8 Importantly, the bed should be associated only with sleep.8
Exercise
Exercise is generally recommended for a healthy lifestyle.8 Some evidence suggests that exercise can be useful in the management of migraine, and low levels of physical activity or a sedentary lifestyle are associated with migraine.8 Based on several studies, the current recommendation for patients with migraine is to engage in graded moderate cardiorespiratory exercise to elicit positive effects.8
Eat
The most consistent food triggers appear to be red wine and caffeine.8 While the benefits of avoiding these specific food triggers is still unclear and controversial, the standard advice for patients with migraine is to consume regular meals.8 A healthy diet with consistent meals, adequate hydration, and low caffeine intake are encouraged; however, they are based on limited studies and are extrapolated from nutrition research.8
Diary
A headache diary is recommended as part of a patient’s headache management.8 Patients can start keeping a headache diary before the initial consultation to assist with diagnosis early in their management. A headache diary includes tracking headache frequency, headache duration, headache intensity, analgesic use, and headache impact on function and absenteeism.8 Physicians and patients generally report improved communication with use of a diary.8
Stress
Many evidence-based techniques for management of stress and mood disorders can also be used in migraine, such as cognitive behavioral therapy, biofeedback, mindfulness, and relaxation techniques.8 Modifications with the highest level of evidence, specifically behavioral techniques, have had the most reproducible results.8 The strongest evidence exists for behavioral management techniques for stress reduction as well as reducing migraine disability, headache severity, and frequency.8
Improving patient involvement, improves patient care
There is a wide range of strategies that migraine patients use to manage their headaches.1 However, poor communication between the clinician and the patient is thought to be one of the underlying causes of migraine under-treatment.1 Gaining insights into clinician‑patient relationships is important to help healthcare professionals better understand the needs of headache patients and to communicate more effectively with these patients.1 Patients’ perceptions of themselves as a resource to manage and make decisions influences their choices in managing their headache.1 Therefore, patient empowerment developed through clinician-patient relationships and shared decision-making can positively impact healthcare outcomes and will likely help shape the future of medical practice.6
Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Migraine and chronic daily headache management: a qualitative study of patients’ perceptions. Scand J Caring Sci. 2004;18(3):294–303.
Dodick DW, Tepper SJ, Lipton RB, et al. Improving Medical Communication in Migraine Management: A Modified Delphi Study to Develop a Digital Migraine Tracker. Headache. 2018;58(9):1358–72.
Park SY, Chen Y. Individual and Social Recognition: Challenges and Opportunities in Migraine Management. ACM Press; 2015. p. 1540–51.
Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE. 2017;12(10):e0186458.
Tornoe B. Children and Adolescents with Primary Tension‐Type Headaches: Research and Practice Perspectives for Non‐ Pharmacological Interdisciplinary Headache Service. InTech; 2017.
Kambhampati S, Ashvetiya T, Stone NJ, Blumenthal RS, Martin SS. Shared Decision-Making and Patient Empowerment in Preventive Cardiology. Curr Cardiol Rep. 2016;18(5):49.
Faizi F, Tavallaee A, Rahimi A, Saghafinia M. Management of Chronic Daily Headache and Psychiatric Co-Morbidities by Lifestyle Modification: Participatory Action Research Combining New Communication Media. Anesth Pain Med. 2017;7(2):e42782.
Robblee J, Starling AJ. SEEDS for success: Lifestyle management in migraine. CCJM. 2019;86(11):741–9.



